กระดูกสันหลัง “เสื่อม” หรือยัง ? สังเกตอาการเบื้องต้นกัน

โรคกระดูกสันหลังเสื่อม เป็นโรคที่สามารถเกิดได้กับใครหลายคน โดยมีปัจจัยมากจากอายุที่เพิ่มมากขึ้น หรือพฤติกรรมการใช้ชีวิตที่ไม่เหมาะสม ซึ่งอาการของโรคสามารถรบกวนการใช้ชีวิตประจำวันได้ หากไม่ได้รับการรักษาที่ถูกวิธี
โดยบทความนี้ จะพาไปทำความรู้จักกับโรคนี้ให้มากขึ้น ไม่ว่าจะเป็น โรคกระดูกสันหลังเสื่อมมีอาการอย่างไร หรือมีแนวทางการรักษาอย่างไรบ้าง หากเป็นแล้วจะรักษาให้หายได้ไหม
Table of Contents
โรคกระดูกสันหลังเสื่อมคืออะไร
โรคกระดูกสันหลังเสื่อม (Spondylosis) คือ ภาวะการเสื่อมของข้อกระดูกสันหลัง โดยข้อกระดูกสันหลังจะประกอบไปด้วย หมอนรองกระดูก (Intervertebral Disc) ซึ่งอยู่ตรงกลางระหว่างตัวกระดูกสันหลังปล้องบนและล่าง ทำหน้าที่เป็นตัวรับน้ำหนัก และข้อต่อ Facet (Facet Joint) ซึ่งจะอยู่บริเวณด้านหลังของกระดูกสันหลัง โดยจะเป็นส่วนที่ใช้ในการขยับก้มเงย หมุน หรือ เอียงตัว โดยเมื่อภาพถ่ายรังสีพบข้อกระดูกสันหลังเสื่อม ผู้ป่วยจะได้รับการวินิจฉัยว่าเป็นข้อกระดูกสันหลังเสื่อม
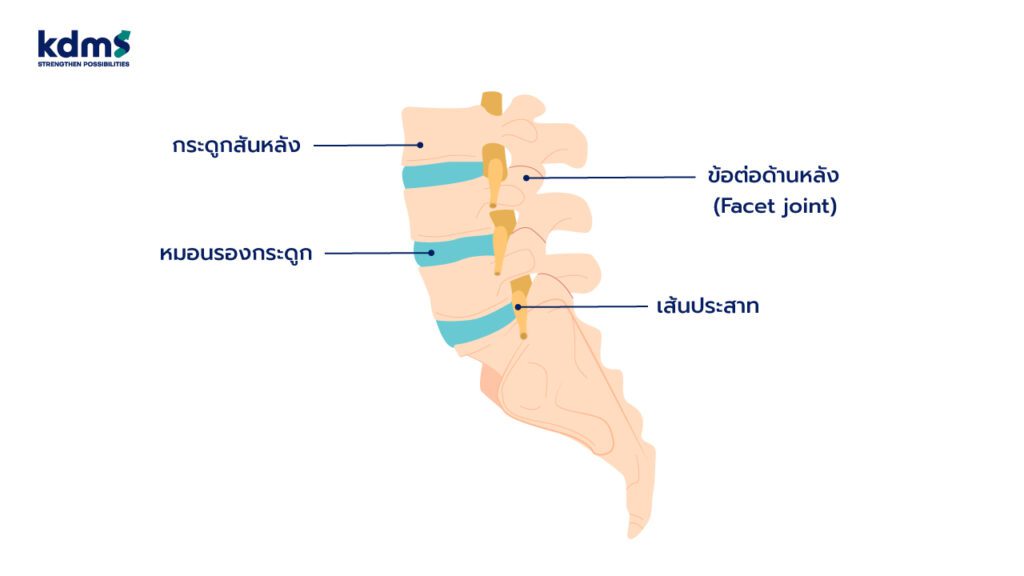
การเสื่อมของหมอนรองกระดูก
การเสื่อมของหมอนรองกระดูกระยะแรก เกิดได้เร็วตั้งแต่อายุ 30 ปี โดยจะเริ่มจากการที่ส่วนประกอบที่เป็นน้ำในหมอนรองกระดูกลดลง ทำให้ความสามารถในการรับน้ำหนักของหมอนรองกระดูกเสียไป ต่อมาอาจเกิดการฉีดขาดของหมอนรองกระดูกด้านนอก และส่วนประกอบที่เป็นเจลที่อยู่ตรงกลางของหมอนรองกระดูกเกิดการเคลื่อนออกมาจากรอยฉีกขาด ทำให้เกิดภาวะหมอนรองกระดูกเคลื่อนกดทับเส้นประสาท (Disc Herniation) ระยะถัดมาเมื่อหมอนรองกระดูกมีการเสื่อมมากขึ้นจะส่งผลให้เกิดหมอนรองกระดูกทรุดตัว โดยจะพบลักษณะในภาพถ่ายรังสี คือ ความสูงของหมอนรองกระดูกเตี้ยลง
การเสื่อมของข้อต่อ Facet
การเสื่อมของส่วนการเสื่อมของข้อต่อ Facet ด้านหลังมักจะเกิดช้ากว่าการเสื่อมของหมอนรองกระดูก โดยเมื่อข้อ Facet มีการเสื่อมระยะแรกส่งผลให้เกิดความไม่มั่นคงในข้อกระดูกสันหลัง โดยถ้าข้อไม่มั่นคงมากจะทำให้เกิดภาวะกระดูกสันหลังเคลื่อน (Spondylolisthesis) ระยะต่อมาร่างกายจะพยายามขจัดความไม่มั่นคงของข้อกระดูกสันหลัง โดยพยายามสร้างกระดูกขึ้นมาเพิ่มเพื่อลดความไม่มั่นคงของข้อต่อ ส่งผลให้พบลักษณะที่เรียกว่า กระดูกงอก โดยกระดูกที่งอกเพิ่มมาจะสามารถทำให้ข้อมั่นคงมากขึ้น แต่ในทางกลับกันกลับส่งผลเสีย คือ สามารถไปกดทับเส้นประสาทได้ ซึ่งเราเรียกว่า กระดูกเสื่อมกดทับเส้นประสาท
สาเหตุของโรคกระดูกสันหลังเสื่อมและลักษณะอาการ

สาเหตุการเสื่อมของกระดูกสันหลังส่วนใหญ่ เกิดจากอายุที่เพิ่มมากขึ้นทำให้เกิดการเสื่อมสภาพของข้อต่อ หรือ หมอนรองกระดูกสันหลัง ส่วนสาเหตุอื่นนอกเหนือจากอายุ ได้แก่ การใช้งานที่มากเกินไป เช่น ยกของหนัก หรือมีการติดเชื้อ หรือ อุบัติเหตุ มาทำลายข้อต่อของกระดูกสันหลัง ซึ่งจะทำให้พบการเสื่อมของข้อต่อในคนอายุน้อยได้ โดยโรคกระดูกสันหลังเสื่อมที่พบได้บ่อย มี 2 ลักษณะ ดังนี้
- ผู้ป่วยกระดูกสันหลังส่วนคอเสื่อม มักจะมาด้วยอาการปวดต้นคอ ปวดสะบัก หรือปวดศีรษะ โดยถ้ามีการกดทับรากประสาท จะทำให้เกิดอาการปวดร้าวลงแขน แขนชา แขนอ่อนแรงได้ แต่ที่อันตราย คือ ถ้าเกิดการกดทับที่ไขสันหลังอาจส่งผลให้เกิดอาการแขนขา อ่อนแรง เป็นอัมพาต การใช้งานมือผิดปกติไม่เหมือนเดิม หรือ การเดินที่ผิดปกติ โดยผู้ป่วยกลุ่มนี้จะเดินช้า ล้มง่าย และขาจะเกร็งแข็ง หรือมีปัญหาต่อระบบขับถ่ายอุจจาระปัสสาวะ
- ผู้ป่วยกระดูกสันหลัวส่วนเอวเสื่อม มักจะมาด้วยอาการปวดหลังด้านล่าง ปวดเมื่อมีการใช้งานแต่พอได้พักอาการปวดจะดีขึ้น ถ้ามีการกดเบียดรากประสาท จะส่งผลให้มีอาการปวดร้าวลงขา ขาชา หรือขาอ่อนแรง ในกรณีที่การกดทับมากขึ้นจนโพรงไขสันหลังตีบแคบ (Spinal Stenosis) จะส่งผลต่อการเดิน โดยจะทำให้ระยะทางที่เดินได้สั้นลง ต้องหยุดพักก่อนที่จะเดินต่อได้ หรือถ้าการกดทับรุนแรงมาก จะส่งผลให้มีผลต่อระบบขับถ่ายอุจจาระปัสสาวะได้
นอกจากนี้ การเสื่อมของกระดูกสันหลัง จะทำให้ผู้ป่วยตัวเตี้ยลงจากหมอนรองกระดูกที่ทรุดตัว และทำให้กระดูกสันหลังเริ่มค่อม และตัวจะโน้มไปด้านหน้ามากขึ้น ซึ่งเป็นภาพที่เห็นได้บ่อยในผู้สูงอายุที่หลังค่อม และเดินแล้วตัวจะโก่งไปด้านหน้า ในกรณีที่ข้อกระดูกสันหลังซ้ายขวาเสื่อมไม่เท่ากัน จะส่งผลให้เกิดการทรุดตัวของข้อไม่เท่ากัน ส่งผลให้เกิดกระดูกสันหลังคดเอียงในผู้สูงอายุได้
โดยสรุป คือ ข้อกระดูกสันหลังเสื่อม ส่งผลกระทบต่อผู้ป่วยทั้งรูปลักษณ์ภายนอก คือ กระดูกหลังคด ค่อม เอียง และ ยังก่อให้เกิดอาการปวดหลังร้าวลงขา ปวดคอร้าวลงแขน อาการชา และอ่อนแรงได้
กลุ่มช่วงวัยใดหรือกลุ่มคนที่มีพฤติกรรมแบบไหนถึงเสี่ยงต่อการเกิดโรคกระดูกสันหลังเสื่อม

ปัจจัยด้านอายุ และพฤติกรรม สามารถส่งผลให้เกิดปัญหากระดูกสันหลังเสื่อมได้ ดังนี้
- ปัจจัยด้านอายุ: หมอนรองกระดูกสันหลังเสื่อมสามารถพบได้ตั้งแต่อายุตั้งแต่ 30 ปีขึ้นไป ส่วนข้อกระดูกสันหลังเสื่อมมักจะพบหลังจากอายุ 40 ปีขึ้นไป โดยความเสี่ยงในการเกิดโรคจะเพิ่มมากขึ้นตามอายุ ซึ่งเป็นปัจจัยที่ไม่สามารถควบคุมได้
- ปัจจัยด้านพฤติกรรม: พฤติกรรมและการใช้งานเป็นสิ่งที่ปรับเปลี่ยนได้ โดยพฤติกรรมที่ส่งผลทำให้ข้อกระดูกสันหลังเสื่อมเร็วได้แก่ การยกของหนัก การนั่งนาน งานที่มีการก้มเงยคอหรือหลังเป็นประจำ น้ำหนักตัวที่มาก การเล่นกีฬาที่มีการสะบัดคอหรือหลังเยอะ กีฬาที่มีการกระแทก การสูบบุหรี่ ปัจจัยเหล่านี้ล้วนมีผลต่อการเสื่อมของข้อกระดูกสันหลัง
อธิบายวิธีการวินิจฉัยโรคกระดูกสันหลังเสื่อมตามลำดับขั้นตอนก่อนรับการรักษา
ก่อนเริ่มการรักษา สำหรับผู้ป่วยที่สงสัยว่ามีอาการกระดูกสันหลังเสื่อม แพทย์จะมีแนวทางในการวินิจฉัย ดังนี้
- การซักประวัติ เริ่มจากการซักถามประวัติ รูปแบบอาการปวด ลักษณะอาการปวด มีอาการปวดร้าวหรือไม่ โดยส่วนใหญ่ถ้าปวดคอต้องระวังเรื่องการปวดร้าวลงแขน ถ้าปวดเอวต้องระวังเรื่องการปวดร้าวลงขา ซึ่งอาการปวดร้าวมักจะแสดงถึงอาการของการกดทับเส้นประสาท อาการชา อาการอ่อนแรง โดยอาการที่สำคัญ คือ อาการเกี่ยวข้องกับปัญหาระบบขับถ่าย เช่น กลั้นปัสสาวะ หรืออุจจาระไม่ได้ ซึ่งบ่งบอกถึงการกดทับเส้นประสาท หรือไขสันหลังที่รุนแรง ซึ่งต้องได้รับการรักษาอย่างเร่งด่วน
- ตรวจร่างกายเบื้องต้น ต่อมาคือตรวจร่างกายเบื้องต้น โดยสังเกตจากลักษณะการเดินของผู้ป่วย ดูจุดกดเจ็บ และ ให้ผู้ป่วยขยับหลัง เพื่อดูท่าทางที่ทำให้เกิดอาการปวด และ ดูการขยับของหลังว่ามีการจำกัดหรือไม่ รวมถึง การตรวจการรับรู้ทางการสัมผัสเพื่อตรวจสอบอาการชา ตรวจสอบกำลังของกล้ามเนื้อในกรณีที่สงสัยการกดทับเส้นประสาท หากพบความผิดปกติ
- ใช้ภาพถ่ายรังสี เบื้องต้นแพทย์จะทำการส่งภาพถ่ายรังสี (X-ray) เพื่อตรวจลักษณะความผิดปกติของข้อกระดูกสันหลัง โดยภาพถ่ายรังสีจะเห็นลักษณะความผิดปกติของกระดูกเป็นหลักเช่น ลักษณะกระดูกงอก ข้อกระดูกสันหลังเคลื่อน หมอนรองกระดูกเตี้ยลง แต่ภาพถ่ายรังสีจะไม่เห็นรายละเอียดของหมอนรองกระดูก และการกดทับของเส้นประสาท
- การตรวจด้วยเครื่องเอ็กซเรย์แม่เหล็กไฟฟ้า (MRI) เป็นการตรวจที่ละเอียดที่สุด และปลอดภัย เนื่องจากผู้ป่วยไม่ได้รับผลกระทบจากการได้รับรังสี เนื่องจากเป็นคลื่นแม่เหล็กไฟฟ้าจึงไม่ส่งผลต่อร่างกาย และยังเป็นการตรวจที่ทำให้แพทย์เห็นรายละเอียดของหมอนรองกระดูก ข้อต่อกระดูกสันหลัง และ การกดทับเส้นประสาทที่ชัดเจนที่สุด
แนวทางการรักษาโรคกระดูกสันหลังเสื่อมมีอะไรบ้าง? ถ้าเป็นแล้วสามารถรักษาให้หายได้ไหม?

แนวทางการรักษาโรคกระดูกสันหลังเสื่อมแตกต่างกันตามความรุนแรงของโรค ซึ่งมีรายละเอียด ดังนี้
- การปรับเปลี่ยนอิริยาบถประจำวัน เช่น หลีกเลี่ยงการก้มเงย การยกของหนัก หลีกเลี่ยงการเล่นกีฬาที่มีการกระแทก ลดน้ำหนัก และหยุดสูบบุหรี่
- การทำกายภาพบำบัด ได้แก่ ประคบร้อน การทำอัลตราซาวนด์ (Ultrasound) การใช้ช็อกเวฟ (Shock Wave) การดึงคอ หรือ ดึงหลัง เพื่อลดอาการปวด รวมถึงการบริหารกล้ามเนื้อเพื่อเพิ่มความแข็งแรงของกล้ามเนื้อหลัง
- ใช้ยาลดอาการปวดและยากลุ่มต้านการอักเสบ การใช้ยาช่วยเพื่อลดอาการปวดตั้งแต่ยาพาราเซตตามอล และยาในกลุ่มต้านอาการอักเสบที่ไม่ใช่สเตียรอยด์ (Nonsteroidal Anti-Inflammatory Drugs) ซึ่งเป็นยาแก้ปวดและลดการอักเสบที่มีประสิทธิภาพที่ดี อย่างไรก็ตาม ต้องระวังเรื่องการใช้ยาที่ต่อเนื่องเป็นระยะเวลานาน เนื่องจากจะมีผลต่อไต
- การฉีดยาสเตียรอยด์เข้าโพรงกระดูกสันหลัง ถ้าอาการไม่ดีขึ้น วิธีถัดมาที่แพทย์จะเลือกใช้ คือ การฉีดยาสเตียรอยด์เข้าโพรงกระดูกสันหลังช่วยลดอาการปวด และการอักเสบของเส้นประสาท (Epidural Steroid Injection) โดยวิธีนี้มีข้อดี คือ ความเสี่ยงต่อการทำหัตถการน้อย แต่ข้อเสียคืออาจจะไม่หาย และตัวยาออกฤทธิ์ได้ประมาณ 3-6 เดือนเท่านั้น
- การผ่าตัด วิธีสุดท้ายที่แพทย์จะแนะนำให้ใช้ในการรักษา คือ การผ่าตัด โดยข้อบ่งชี้ของการผ่าตัด ได้แก่ อาการไม่ตอบสนองต่อการรักษาข้างต้น มีอาการอ่อนแรงของกล้ามเนื้อแขนหรือขา มีความผิดปกติต่อระบบขับถ่ายอุจจาระปัสสาวะ
วิธีการปฏิบัติตัวของผู้ป่วยกระดูกสันหลังเสื่อมหลังรับการรักษา
ผู้ป่วยจะต้องปรับเปลี่ยนพฤติกรรมการใช้ชีวิต หลีกเลี่ยงการยกของหนัก หลีกเลี่ยงการก้มเงยหลังมากๆ ลดน้ำหนัก ลดการสูบบุหรี่ และผู้ป่วยควรต้องฝึกบริหารกล้ามเนื้อแกนกลาง (Core Muscle Strengthening) ได้แก่ การบริหารกล้ามเนื้อคอ กล้ามเนื้อหน้าท้อง และ กล้ามเนื้อหลัง
การป้องกันหรือหลีกเลี่ยงโรคกระดูกสันหลังเสื่อม

การปฏิบัติตัวเพื่อป้องกันและลดความเสี่ยงในการเกิดโรคกระดูกสันหลังเสื่อมสามารถทำได้มากมาย เช่น
- การนั่งในท่าที่เหมาะสม นั่งในท่าที่ดี หลังตรง มีการพักเพื่อยืดเหยียดเป็นระยะ
- ไม่ทำกิจกรรมในท่าใดท่าหนึ่งเป็นเวลานาน
- ออกกำลังกาย เพื่อเพิ่มกล้ามเนื้อบริเวณหลัง
- หลีกเลี่ยงบางพฤติกรรม เช่น การยกของหนัก ก้มๆ เงยๆ
- ระมัดระวังอุบัติเหตุ ที่มีการกระเทือนต่อกระดูกสันหลัง
โรคกระดูกสันหลังเสื่อม คือ ภาวะการเสื่อมที่เกิดกับส่วนประกอบของข้อกระดูกสันหลัง อย่าง หมอนรองกระดูก และข้อต่อ Facet ซึ่งสามารถก่อให้เกิดได้กับผู้สูงอายุ หรือกลุ่มคนที่มีพฤติกรรมไม่เหมาะสม เช่น นั่งท่าเดิมนานๆ หรือยกของหนักเป็นประจำ โดยผู้ป่วยอาจมีอาการปวดในบริเวณใกล้เคียง หรืออาจมีอาการแขนหรือชา หากมีการกดทับที่เส้นประสาท เมื่อเกิดความผิดปกติต่างๆ ขึ้น จึงควรรีบพบแพทย์ เพื่อให้วินิจฉัย และเลือกวิธีการรักษาที่เหมาะสม ซึ่งจะช่วยให้ผู้ป่วยสามารถกลับมาใช้ชีวิตได้อย่างเป็นปกติ


 history
history  appointment
appointment 




 451,000* บาท
451,000* บาท
 สิ้นสุด 30/06/2024
สิ้นสุด 30/06/2024 












